(content note: scientific discussion of depression & suicide)
"Too Long; Didn't Read" Summary:
Exactly what the title says.
Longer Summary:
The "effect size" of the best antidepressants on depression, vs placebo, is around 0.4. (On average; some people respond much better or much worse.) This is like going from a C to a C+.
In contrast: the effect size of 1500 mg/day of "≥60% EPA" Omega-3 supplements is a bit higher, around 0.6. This is like going from a C to a B–. (With uncertainty; at worst, Omega-3's "only" on par with antidepressants.)
But, much better: the effect size of 4000 IU/day of Vitamin D is twice as high as antidepressants', around 1.0. This is like going from a C to an B! (With uncertainty; at worst, Vitamin D's "only" on par with antidepressants.) This works even for people who don't have a Vitamin D insufficiency — but around half of American adults do.
(edit Feb 5: after diving deeper into the research, I'm less confident in Omega-3, but a bit more confident in Vitamin D. Reader take notice!)
Even if you're already taking Vitamin D & Omega-3, double check your dose: it may still not be enough! The official recommendations are all too low, and recent research suggests even the official maximum safe dose for Vitamin D is too low.
I know the "yay supplements" genre of writing is full of sloppy research & grifters, and you should be skeptical of my claim of easy wins, of "$100 bills laying on the sidewalk". But there is good science among the trash, and policy is often decades behind science in any field, not just health.
(Also, note I'm NOT saying "take vitamins instead of antidepressants"; the research shows these interventions can be stacked! You can supplement meds with, well, supplements. And of course, depression is not "just" chemistry — but it's not just not-chemistry, either.)
So, Vitamin D & Omega-3: possibly high reward, for low risk. That's a positive "expected value" bet! These supplements are mostly safe, cheap, and over-the-counter. As always, "ask your doctor", show them the peer-reviewed papers cited in this post.
Unless you have specific reasons to not take Vitamin D & Omega-3 — kidney stones, blood thinners, etc — please try them, for at least a month! They could save your mental health. Maybe even your life.
Confidence level: I read the existing meta-analyses, but I have not (yet) done a full meta-analysis myself. I'm not an expert in nutrition, I'm just a stats-literate person who wants to figure out what's best for myself & my loved ones.
Table of Contents:
- A crash course in "effect sizes" ↪
- Interpreting effect sizes on depression ↪
- Antidepressants (& two cheers for "placebo") ↪
- Omega-3 ↪
- Vitamin D ↪
- Conclusion: All this time, you lacked the Vitamin? ↪
Post-publication edits:
- Jan 29th: #2 on the Hacker News frontpage! Thank you for your feedback, I spent all day editing this post, incorporating the constructive criticism & adding details. Also: the intended tone of this post is, "what makes science awesome is that it's self-correcting, finding mistakes in older science is good, here's how the older science was mistaken", not "f@#$ science". Also 2: thank you Josep for catching my medically disastrous typo.
- Jan 30th: MAJOR edit: I downgraded high-dose Vitamin D's effect from 1.8 to 1.0, and my recommendation from 5000 IU/day to 4000 IU/day. My mistake was not applying a more reasonable "prior probability". So, instead of being 4 times better than antidepressants, I now estimate it's "only" 2 times better. Either way, I'm still confident the title of this post holds: high-dose Vitamin D is as good or better than the best antidepressant.
- Feb 5th: A few more details. Much less confident in Omega-3, a bit more confident Vitamin D's at least as good as antidepressants.
A crash course in "effect sizes"
In Alicetown, the average person has 4 younger cousins.
In Bobtown, the average person has 3 younger cousins.
Alright, not so surprising. You may not even notice a difference.
In Alicetown, the average person has 4 limbs.
In Bobtown, the average person has 3 limbs.
You'd definitely notice.
It's the same absolute difference (4 vs 3) and relative difference (3/4). So what makes limbs more surprising than cousins? Well, partly it's more dramatic & visible, but also because: we expect high variation in the number of someone's younger cousins, but not their number of limbs.
This is why scientists calculate an "effect size" or "standardized mean difference" ("mean" = average). We take the difference between two groups, then divide by the total amount of variation, to account for how surprising a difference is.
(This is a health article, not a math article, so I'll skip the formulas in this post. If you're curious, : check out this 4 min video.)
Unfortunately for laypeople, the effect size is usually just reported as a number, like "+0.74" for spacing out your studying vs cramming, or "–0.776" for sleep deprivation on attention.
But what's that mean? How can we make these numbers intuitive?
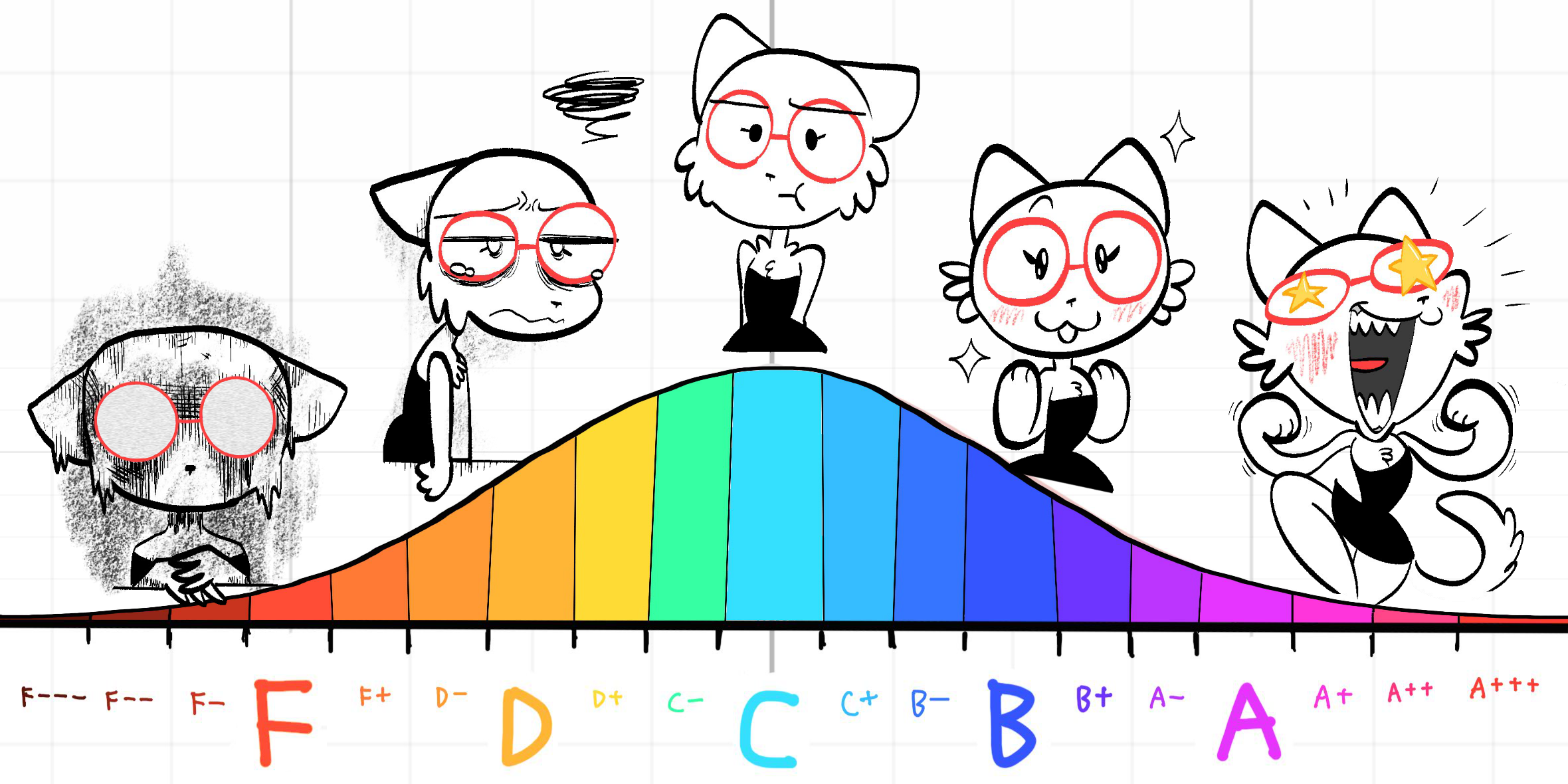
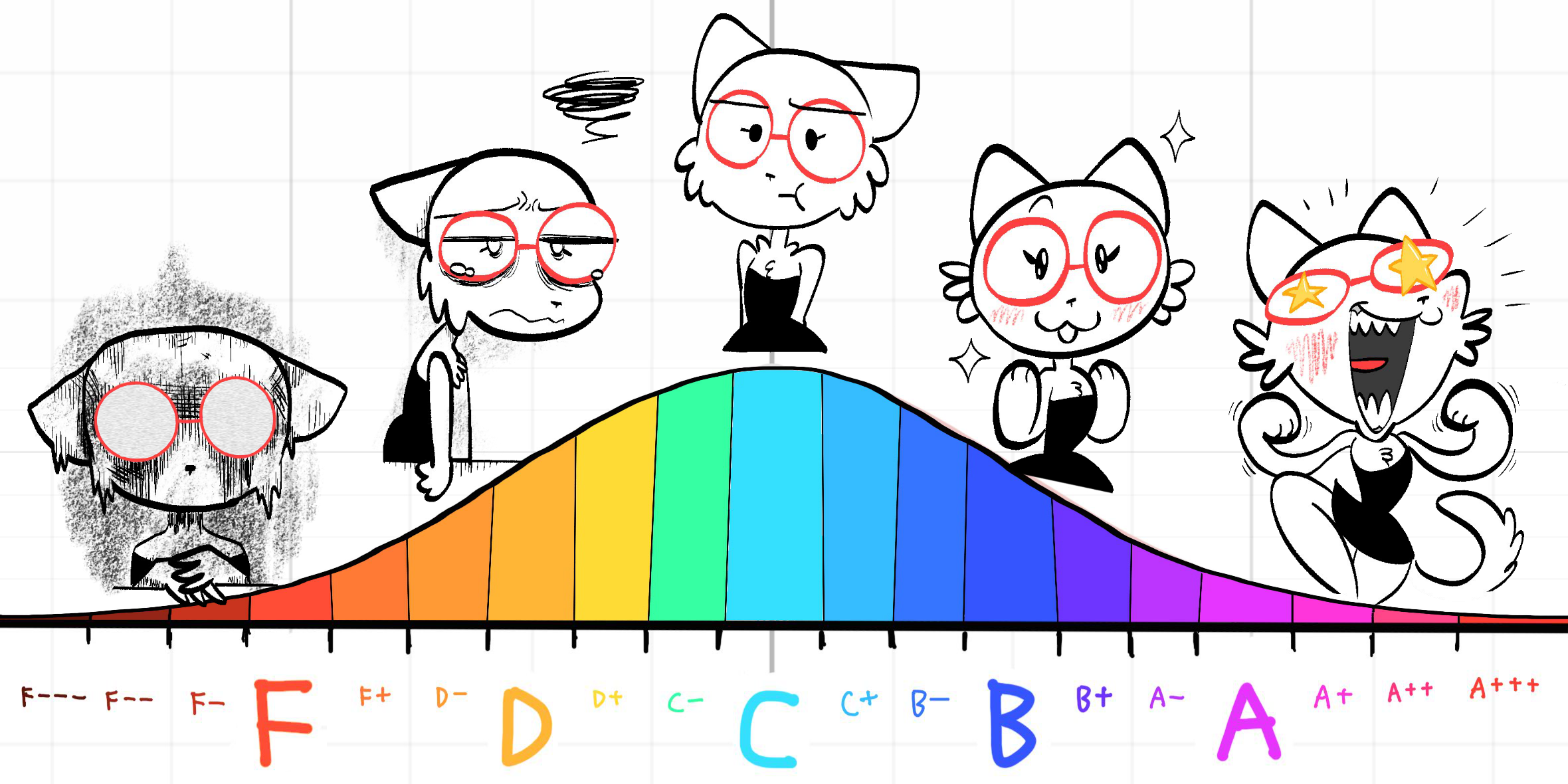
Well, a common way for data to be is a bell-shaped curve (also called a "normal distribution"). And most of us are, alas, well-acquainted with the bell curve in school grades. ("grading on a curve")
So: school grades give us a useful way to think about standardized effect sizes! We can now convert that number into an actual letter grade:
- F: -2.0 below average
- D: -1.0 below average
- C: average
- B: +1.0 above average
- A: +2.0 above average
(see footnote for more precise ranges.[1] the units are in "standard deviations", or "sigmas". what's sigma? sigma ba-- just a unit of "how far away this is from average, relative to the total variation".)
For example: spacing out your studying, relative to cramming, will on average lift your test scores from a C to a B–. (effect size = +0.74) And short-term sleep deprivation, relative to healthy sleep, will on average tank your ability to pay attention from a C to a D+. (effect size: –0.776)
(Note — when reading about effect sizes, always remember: effect of what, on what, at what dose, for which group, relative to what? See the Data Colada post, Meaningless Means.)
(Note 2 — the standard way of "intuitively" describing effect sizes is Cohen's recommendations: 0.2 = small, 0.5 = medium, 0.8 = large. Personally, I prefer the "school grade letter" comparison, since it's more concrete. But hey, you do you.)
But it's not limited to just grades & academic performance. Effect sizes can also help us understand any kind of difference between groups, in observation or in experiments!
For example...
Depression!
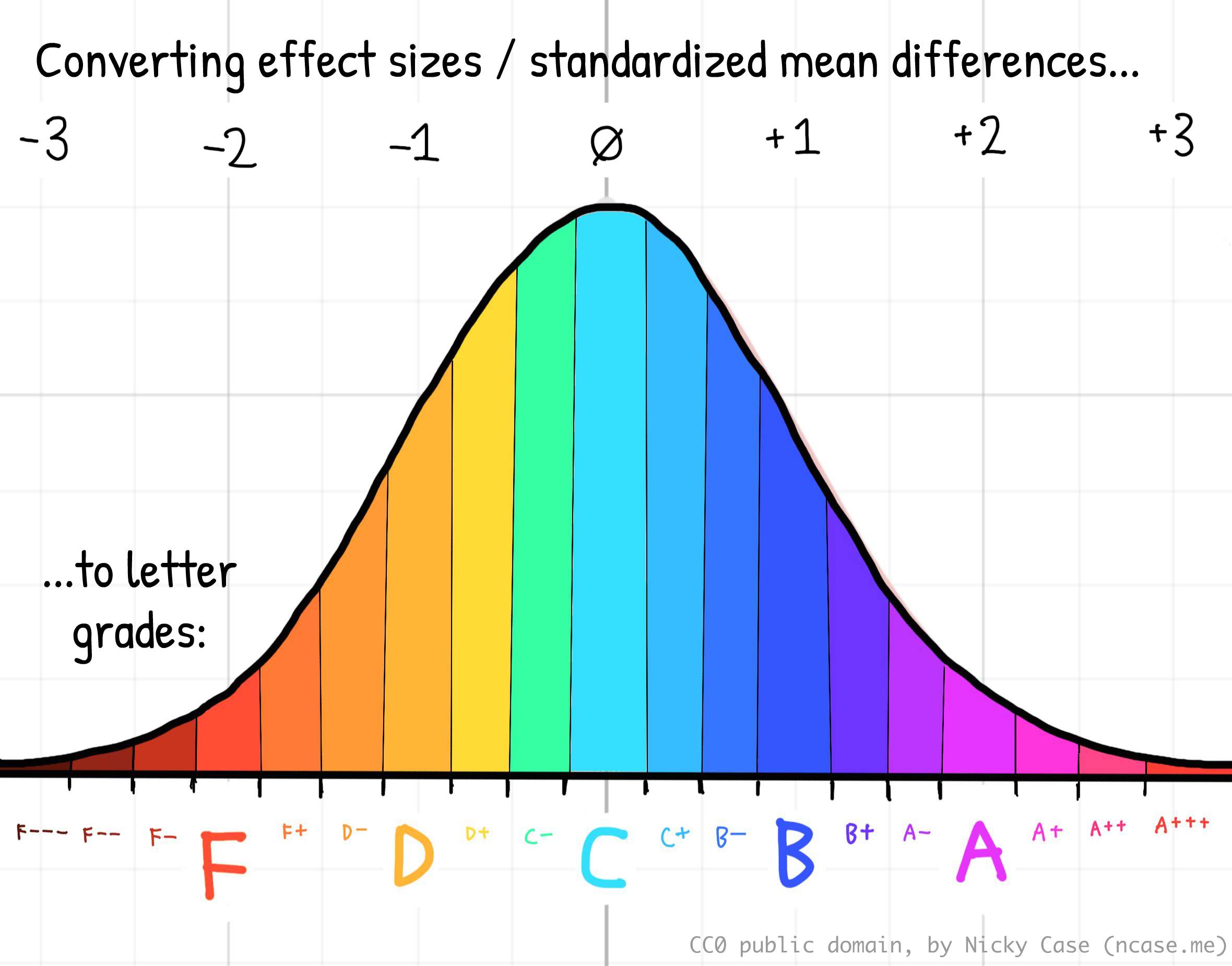
Let's use our school grade analogy, to interpret effect sizes on mental health:
What's an "F in mental health"? By definition of a bell curve, ~2.3% of people are below –2 sigma (an "F"). (See: this bell curve calculator.) In Canada, ~2.6% of people had suicidal ideation in 2022, while in the US, it was ~4.9% in 2019. So, it's not too far off to say: "F in mental health = literally suicidal". (Also, reminder that ~4% is 1-in-25 people. You likely know someone, or are someone, who will feel suicidal this year. Please reach out to your friends & loved ones!)
What's a "D in mental health"? ~16% of people are below –1 sigma (a "D") on a bell curve. The Keyes 2002 study estimated that ~14.1% of adults meet the DSM-III criteria for a major depressive episode. So, D = Depressed.
What's an average "C in mental health"? ~68% of people are within a sigma of average (a "C") on a bell curve. Same above study found that 56.6 percent had moderate mental health. They were neither "languishing" nor "flourishing". I guess C = Could Be Worse.
What's a "B in mental health"? ~16% of people are above +1 sigma (a "B") on a bell curve. Same above study found that 17.2% of adults are "flourishing". Good for them! B = Flourishing, life is good.
What's an "A in mental health"? I don't know who these freaks are. I actually could not find any scientific studies on "the +2 sigma in well-being". In contrast, there's lots of research on suicidal ideation, the –2 sigma in well-being. In the absence of any actual data, I'll just say: A = AWESOME
So, if an intervention is found to have an effect size of +1.0, that's like going up a letter grade. If something's found to have an effect size of -2.0, that's like going down two letter grades. And so on.
Okay, so how do we get peoples' "mental health grades" up?
Let's look at antidepressants, Omega-3, and Vitamin D, in turn:
Antidepressants
The good news is they work. The bad news is they don't work as well as you'd think they may work.
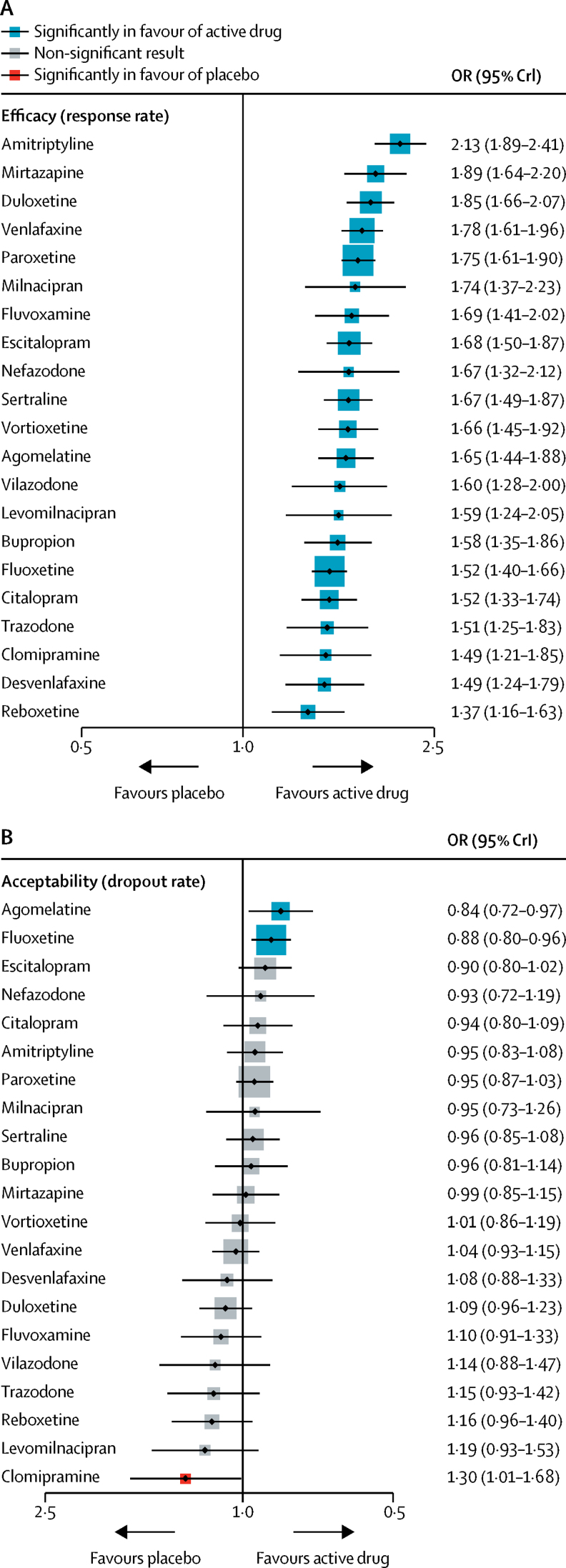
Cipriani et al 2018 is a meta-analysis: a study that collects & combines lots of previous studies (that pass some basic criteria, to minimize a garbage-in-garbage-out situation). While meta-analyses aren't perfect, it's usually better for "science communicators" like me to cite meta-analyses over individual studies, to reduce the chance I'm cherry-picking.
Anyway: this meta-analysis analyzes 522 trials with 116,477 participants → over 200 participants per trial, on average. All 21 antidepressants they studied were better than placebo (a pill that contains no active medicine). The most effective antidepressant, Amitriptyline, had an "Odds Ratio" of 2.13, which converts to an effect size of 0.417, which is "small-medium" according to Cohen's recommendations. Or, by our school-letter-grade comparison: the best antidepressant would take your mental health grade from an F to F+, or C to C+.
(Meanwhile, the median antidepressant's effect size is lower, around 0.28.[2])
From Figure 3 of that paper, you can see that Amitriptyline has the highest estimated effect size, while the side effects are no worse than placebo:
But hang on, only F to F+ on average? How does that square with people's personal experience that antidepressants have been lifesaving?
Well, first: the average person has around 1 testicle.
The punchline being ~50% of people have 2 testicles while ~50% of people have 0 testicles, hence the average is "around 1". Likewise, the average effect for the best antidepressant is 0.4 — but some people respond much better than that... and some respond much worse. (e.g. different kinds of antidepressant, different kinds of depression, different kinds of people, etc. Note that this caveat also applies to the Vitamin D & Omega-3 studies, and all medical studies.)
And, second: the belief that things will get better is a powerful thing. Unfortunately, the power of hope gets a bad name in medicine: "placebo".
When you take any medicine, you don't just get (effect of medicine). You get (effect of medicine + effect of placebo + effect of time).
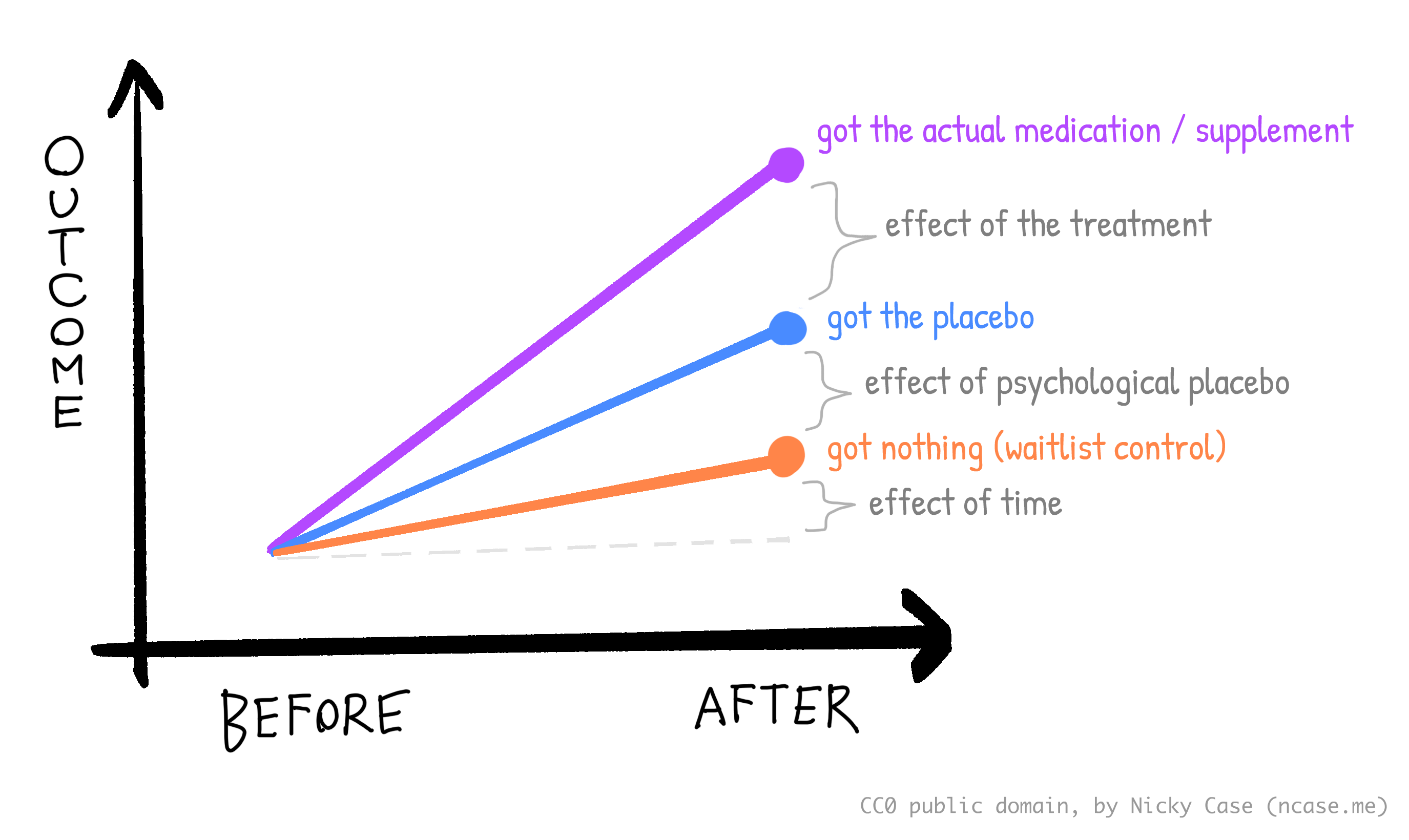
The effect of placebo + time: probably around 0.9.[3]
The effect of placebo alone: Amazingly, despite researchers having used placebos for decades, it's only recently that we started testing "open-label" placebos: placebos where we just tell the patient it's a placebo. We then compare "getting placebo" to "getting nothing". The effect size of open placebo, on stuff ranging from pain to depression, is around 0.43. (Spille et al 2023)
The effect of time alone: Using the above two numbers, I'd guesstimate: 0.9 - 0.43 = 0.47. "Time" includes both natural healing, and "regression to the mean".
So, the individual effect of medication, psychological placebo, and time, are all around +0.4 each. And combined, they give you +1.20, or going from F to D+ or C to B+. That's why many people report antidepressants being lifesaving! (Again, on average; some people react much worse.)
"Wait, the improvement from antidepressants is mostly placebo + time?" Yes, and this is widely known in psychiatry. I mean, they're not yelling it from the rooftops, but this has been an established consensus fact for decades. The infamous Kirsch & Sapirstein 1998 first estimated that the improvement from antidepressants is ~75% placebo + time, and later better meta-analyses have replicated this result. Even the most critical response to Kirsch's work, Fountoulakis & Möller 2011, still finds it's mostly placebo + time.[4]
But again, I think "placebo" is too dismissive a word for the power of hope. Hope isn't magic, but it's something, and measurably so: around +0.4. I assert: the placebo effect isn't a bug, it's a feature! It proves the connection between mental state & physical health.
(The recent discovery of open-label placebos, is also an example of how there's still low-hanging fruit — "$100 bills on the sidewalk" — even in modern medicine! I hope that makes it more plausible to you, that Vitamin D & Omega-3 really could be overlooked, high-impact interventions.)
But anyway, for the rest of this article, I'll only be reporting effect sizes versus placebo + time. Just remember that the power of hope gives you an extra +0.4 (like C to C+) for all interventions.
Omega-3
Keep getting confused on which fat is what? Me too. So, here's a crash course on various fats:
Fatty acids are chains of carbons & hydrogens + two oxygens. They say "OOH" at one end, and "HHH" at the other end:
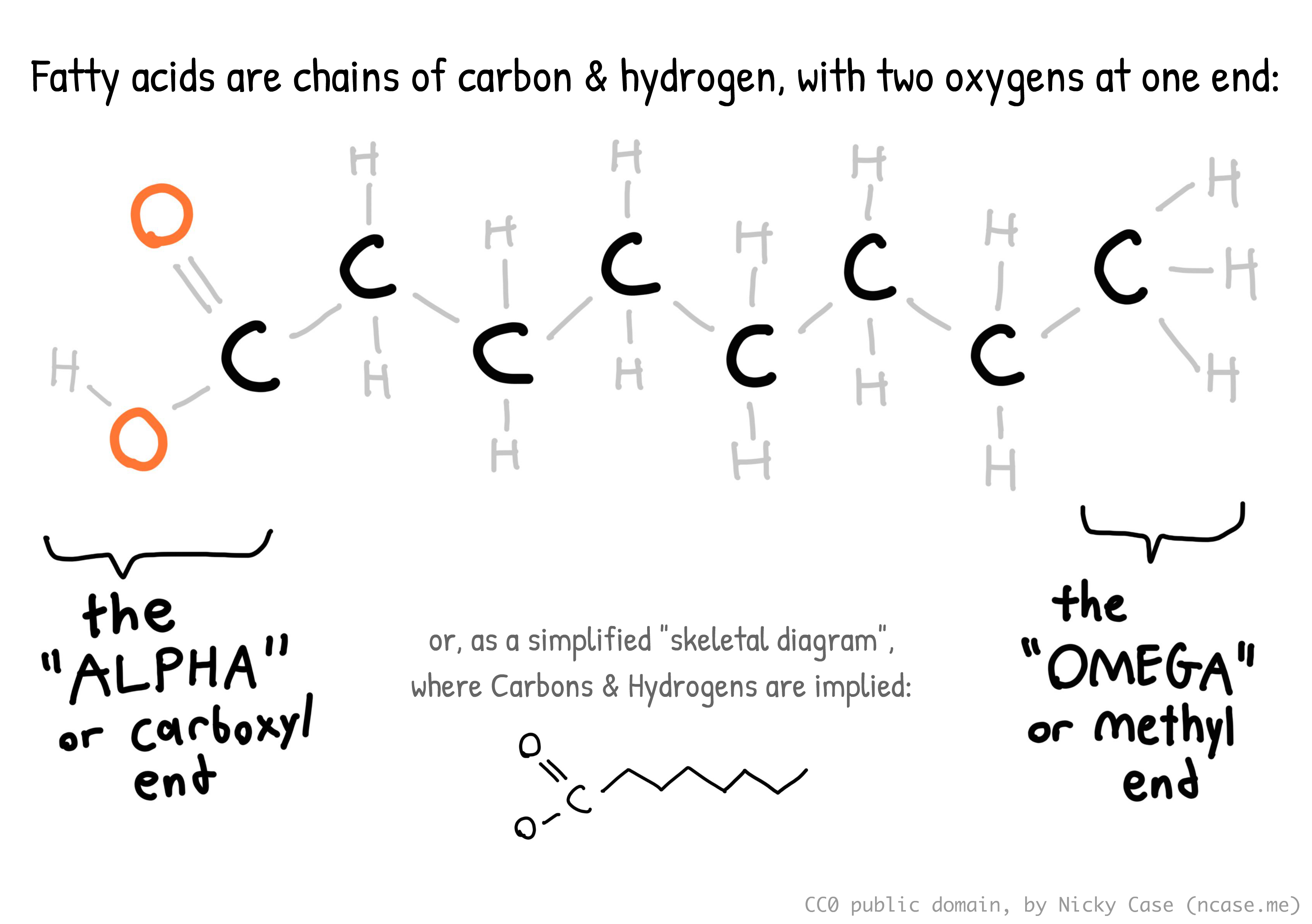
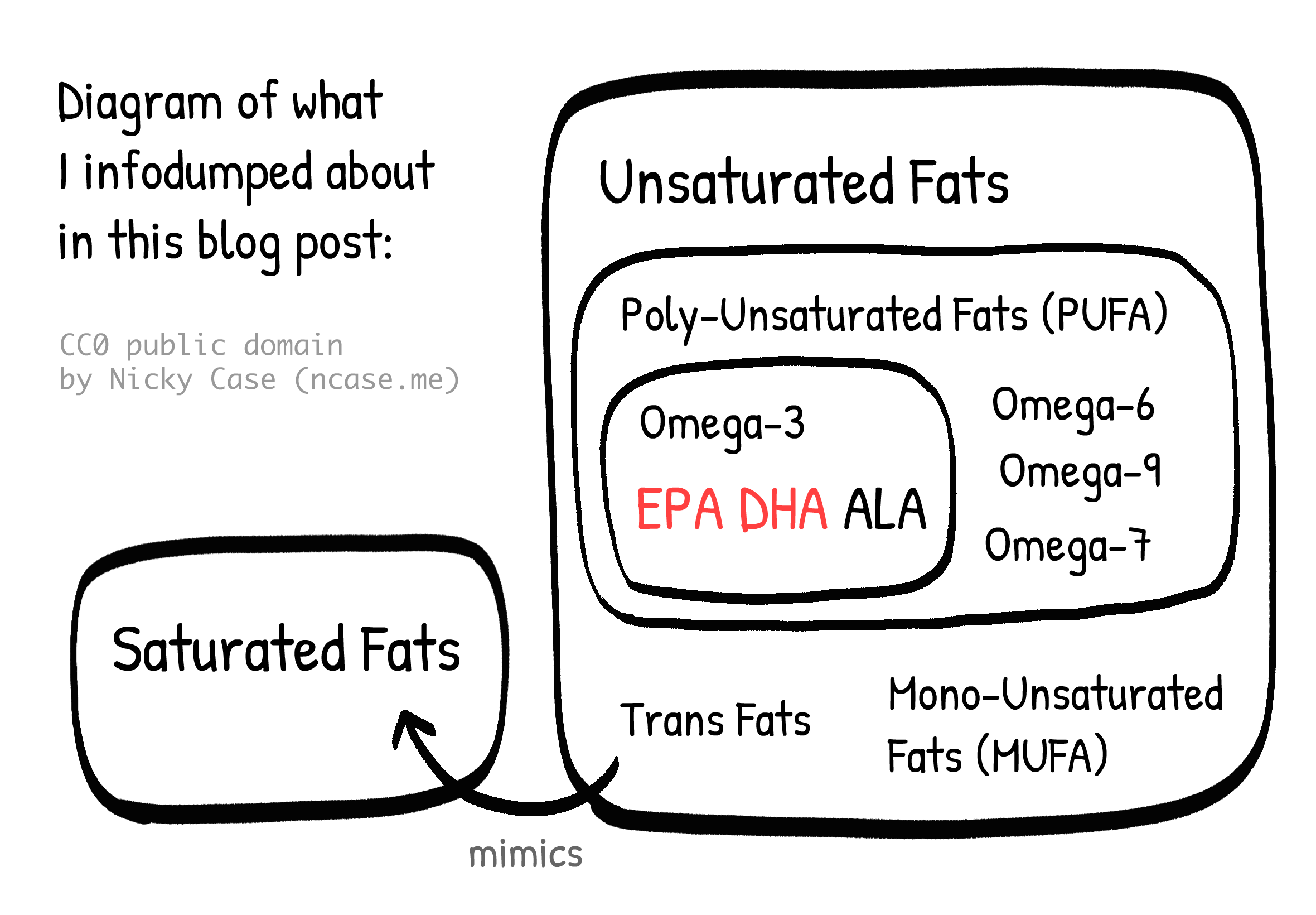
A saturated fatty acid is one where all the carbons' free spots are filled up with hydrogens. (Hence, "saturated") This makes the molecule stick straight out. This is why long saturated fatty acids — like those found in butter — tend to be solid at room temperature.
(Contrary to popular belief, saturated fats don't literally clog your arteries, like grease in plumbing pipes. What happens is {ha ha I don't actually understand this}. Something about your cholesterol levels & inflammation.)
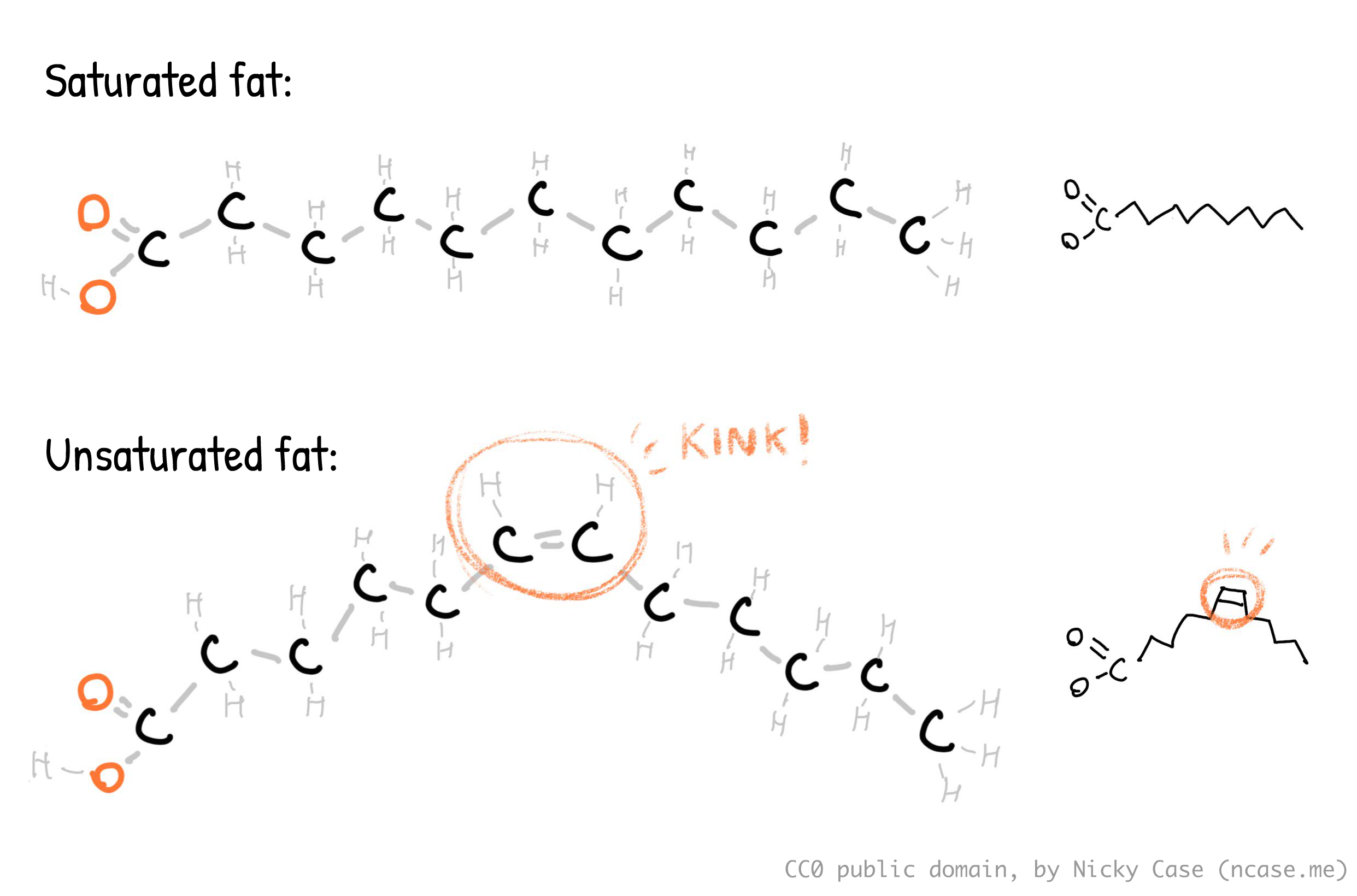
In contrast, unsaturated fatty acids have at least one hydrogen missing. This causes them to have a double-bond "kink" in the molecule. This makes them not stick out, which is why unsaturated fats tend to be liquid at room temperature. Mono-unsaturated fatty acids (MUFAs) — like in olive oil — only have one kink. Poly-unsaturated fatty acids (PUFAs) — like in fatty fish — have two or more kinks. Let's be mature adults about this, please.
For completeness: trans fats are unsaturated fats whose "kink" is twisted around, causing them to go straight. That is the worst sentence I've written all month. The twisted kink is caused by the hydrogens being on opposite sides, hence "trans". (And yes, if they're on the same side it's "cis". Latin was a mistake.) The molecule being straight is why trans fats — which margarine used to be full of — are solid at room temperature, despite being an unsaturated fat.
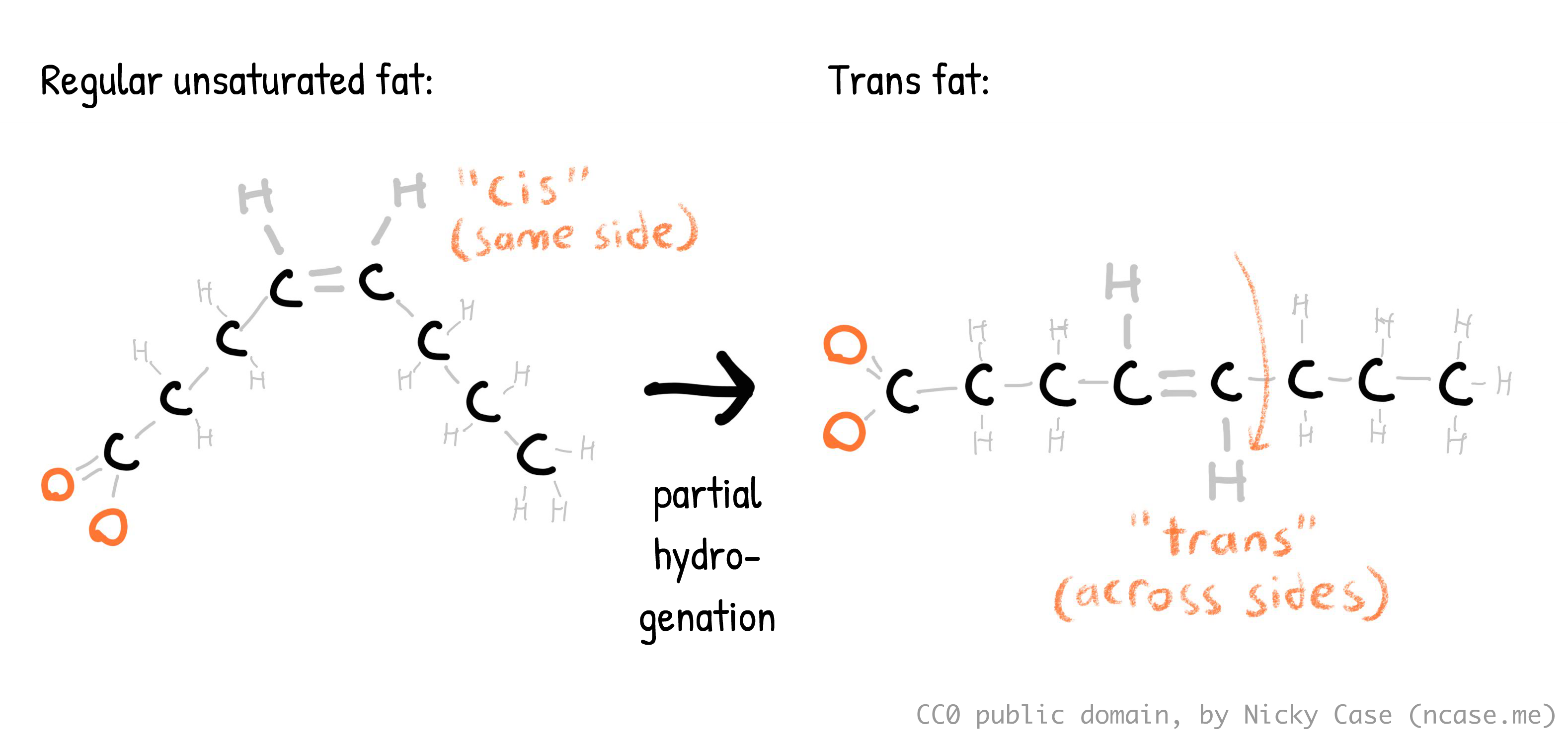
It's neat whenever you can trace the history of something right down to its atoms! Margarine was first invented because it's cheaper, and is spreadable straight from the fridge, unlike butter. Margarine (used to be) made by taking unsaturated vegetable oils, which were cheaper than animal fats, then pumping a bunch of hydrogens into it (hence, "hydrogenated oils"). If you completely hydrogenate an oil, it becomes a saturated fat. But they only partially hydrogenated those oils, leading to trans fats, which were cheaper & a spreadable semi-solid at fridge temperature.
In the 1970s & 80s, the US Food & Drug Administration concluded that trans fats were not harmful to humans, and nutritionists promoted margarine over butter, because butter had "unhealthy" saturated fats. But in the early 1990s, scientists realized that trans fats were even worse for you than saturated fats. Only in the 2010's, did most Western countries start officially banning trans fats. Reminder: policy is often decades behind science.
(Hey, what do you call it when you get thiccer on HRT? Trans fat! :D)
I need to stop going on infodump tangents. Anyway, Omega-3 is any fatty acid with its first kink at the 3rd carbon from the Omega end ("HHH"), though it can have more kinks later down the chain. (And yes, Omega-6 has its first kink at the 6th carbon, and Omega-9 has its first kink at the 9th carbon. There's nothing physically preventing Omega-4 or Omega-5's from existing, but due to some quirk of evolution, Omega-3, -6, and -9 are the ones biological life uses most. As far as I can tell, there's no specific reason they're all multiples of 3. Probably just a coincidence. There is a less common Omega-7.)
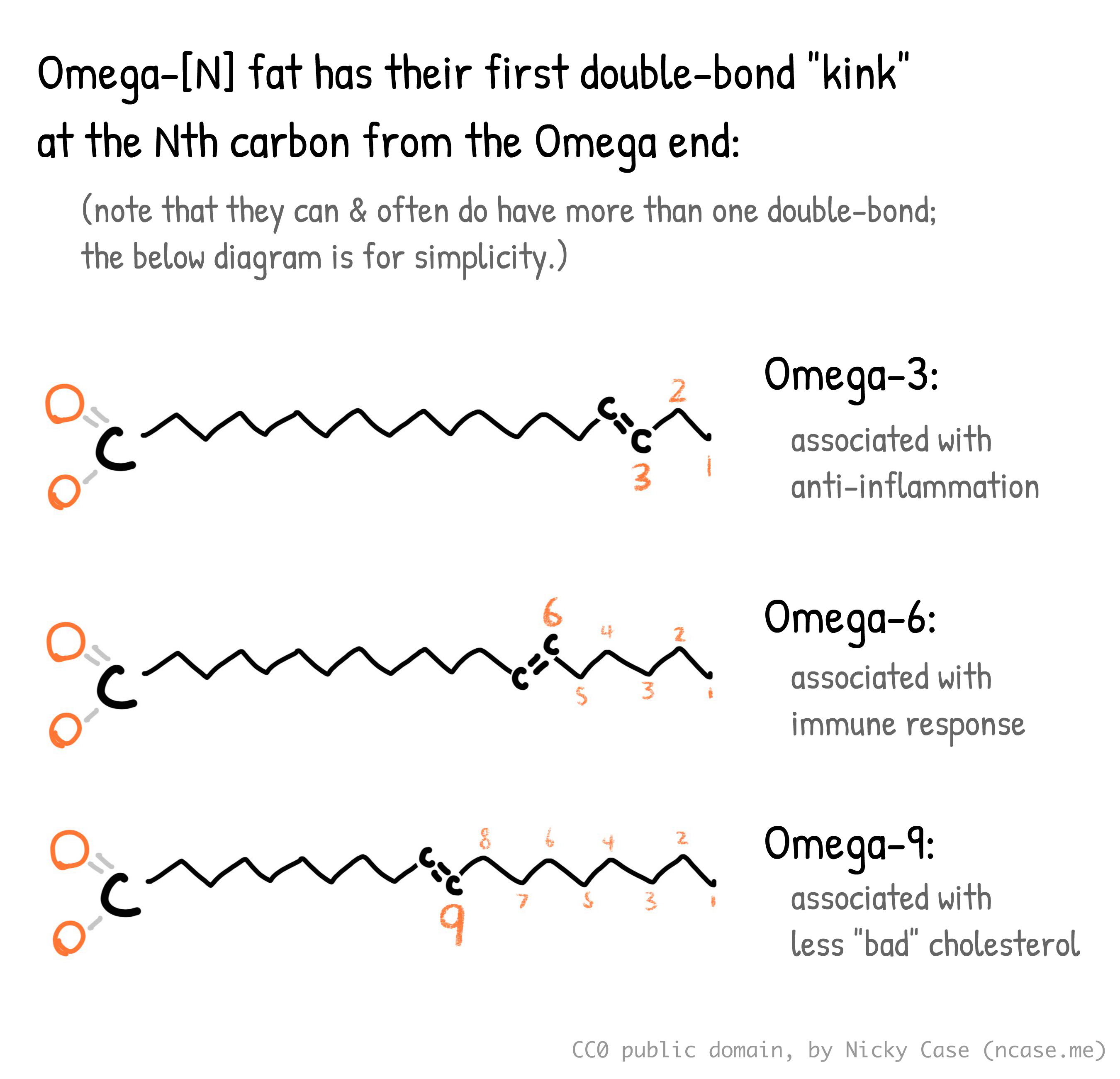
Finally, there's three main types of Omega-3: EPA (Eicosapentaenoic Acid), DHA (Docosahexaenoic Acid), and ALA (Alpha-Linolenic Acid). ALA is mostly found in plants like chia seeds & walnuts, while EPA & DHA mostly come from seafood, though there are algae-based vegan sources.
(Figure 1.1 from Roke 2016.⤵ Thank you Kaitlin Samantha Roke for drawing this coz I'm too lazy to draw it myself. Note how the first double-bond "kink" for all these molecules is at the 3rd carbon from the Omega end — hence why they're all called Omega-3's.)
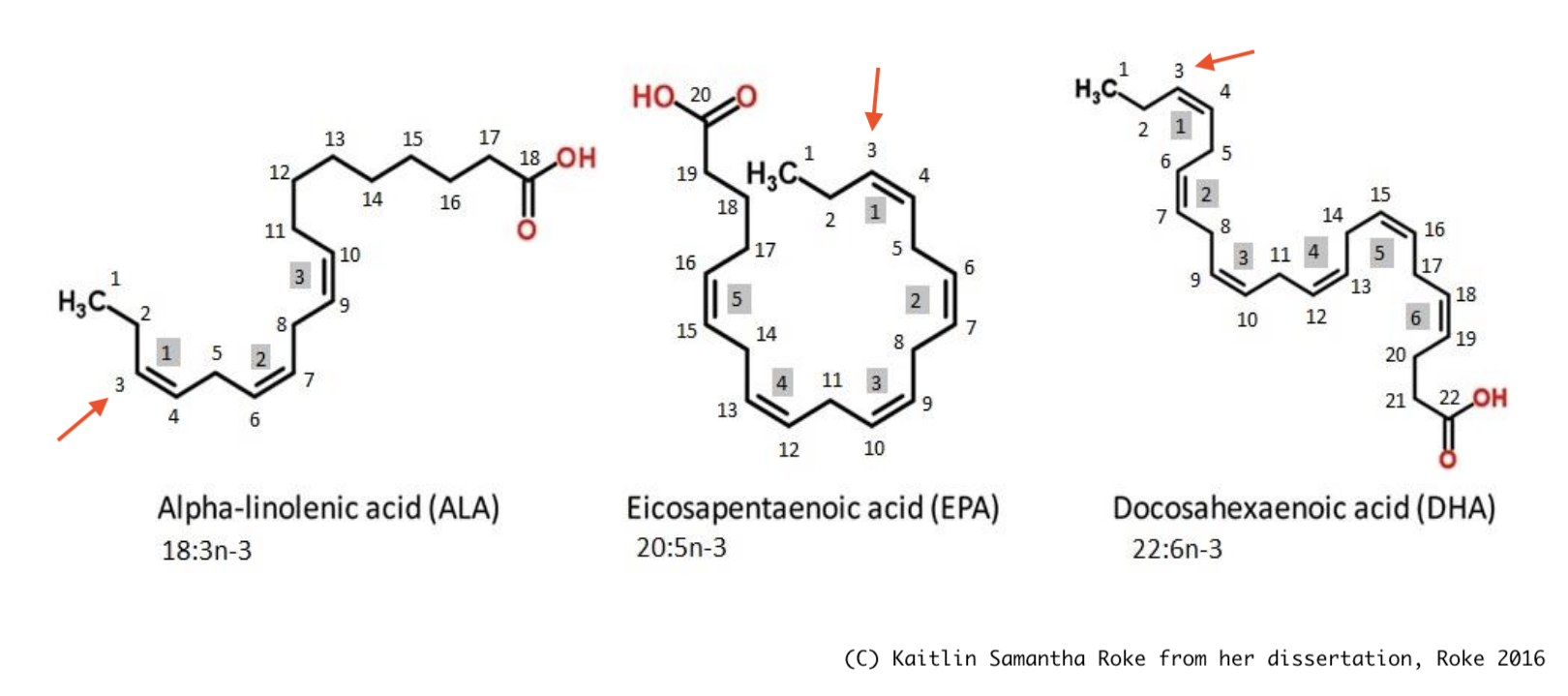
EPA & DHA are the focus of this section. For bio-mechanical reasons I don't understand but I assume someone else does: EPA is the one associated with anti-inflammation, better brain health, and less depression... while DHA isn't. (But DHA is still needed for other stuff, like your neurons' cell walls, so don't cut them out completely!)
(Note: I could not find any experimental trials of ALA on depression, though an observational study in Japan (Kurotani et al 2014) finds a correlation between higher ALA and lower depression. But reminder, correlation is not necessarily causation.)
All the above info in a Venn (technically Euler) diagram:
Okay, enough yap. Time for the actual data:
Sublette et al 2011 is an older meta-analysis (15 trials with 916 participants → 61 participants per trial, pretty low to be honest). But this was the only meta-analysis I could find that estimates the actual "dose-response" curve, which shows: how much effect, for how much treatment.
Why is dose-response important? Because one problem with many meta-analyses is they'll do something like: "Study 1 gave patients 1 gram of medicine and saw a +1 improvement in disease, Study 2 gave 10 grams and saw +4 improvement, Study 3 gave 100 grams and saw negative –5 improvement… the average of +1, +4, and –5 is zero... therefore the medicine's effect is zero."
As mentioned earlier, this is a meaningless mean. That's why we want to know the response at each dose.
Anyway, the Sublette meta-analysis gathered randomized trials studying Omega-3 on depression (vs placebo, of course) and got the following dose-response curve.⤵ Note that the horizontal axis is not just amount of total Omega-3, but specifically the extra amount of "unopposed" EPA, above the amount of DHA. Or in other words, "EPA minus DHA":
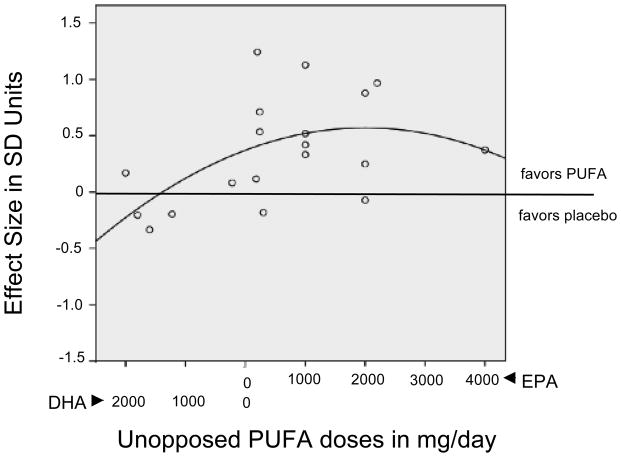
The top effect size is around +0.558, which is like going from an F to D–, or C to B–. You get this maximum effect around 1 to 2 grams of extra EPA, and too much EPA gets worse results. The meta-analysis finds that Omega-3 supplements that are ~60% EPA (and the rest DHA) are optimal.
(Though, honestly, I'd ignore the fitted upside-down-U curve in the above figure, and just look at the dots, the raw data. The main signal seems to be "If mostly EPA then it's good, if mostly DHA then no effect".)
Is this in line with later meta-analyses? More or less! Liao et al 2019 also finds that ~1 gram of ≥60% EPA is best, but actually finds a higher effect size: +1.03. Kelaiditis et al 2023 also finds 1 to 2g of ≥60% EPA is best, but found a lower effect size of +0.43… which is still as good as the best antidepressant! So, I'm taking +0.558 as the median estimate.
(Note that when the meta-analyses report the "average" study's effect size, this includes mostly-DHA and low-dose Omega-3. The effect sizes I bolded above are for ≥60% EPA at high doses.)
Yes, it is concerning that several meta-analyses of the same scientific literature can return vastly varying estimates. More high-quality studies are definitely needed. That said, even the lowest estimate is on par with the median antidepressant, which has an effect around +0.28.
Is there "publication bias"? One popular critique of supplement studies is that the effect is inflated, because studies that find low to no effects don't get published. But if this was the case, we should see gaps & asymmetry in the data. Do we? Admittedly, yes: Sublette 2011 & Kelaiditis 2023 finds publication bias, but Liao 2019 doesn't. These meta-analyses had different criteria for which studies they accepted or not.
Let's convert this to an actionable recommendation: There's a lot of uncertainty, but the only thing the above meta-analyses agree on is "60% or above EPA" and "somewhere between 1 and 2 grams". So let's just say: get 1500 mg/day of 60%-EPA Omega-3 supplements.
In comparison, most official health organizations recommend "250–500 mg combined EPA and DHA each day for healthy adults." That is over three times too low, at least for optimal effects on depression, which we estimated is around 1500 mg/day. (The official maximum safe dose is 5000 mg/day)
Direct effect on suicide: Finally, a (small) study directly investigating the link between suicide & Omega-3. Sublette et al 2006: “Low [DHA] and low Omega-3 proportions [...] predicted risk of suicidal behavior among depressed patients over the 2-year period.” Though keep in mind this is a small study, and it's observational not experimental. Also, weird that contrary to the above studies on depression, DHA predicted suicide but not EPA. Not sure what to make of that.
Bonus: Omega-3 may also boost cognition? Shahinfar et al 2025: “Enhancement of global cognitive abilities was observed with increasing omega-3 dosage up to 1500 mg/day. [effect size = 1.00, like going from a grade of C to B!], followed by downward trend at higher doses.”
Vitamin D
Ghaemi et al 2024 is a meta-analysis on Vitamin D on depression. (31 trials with 24,189 participants → over 700 participants per trial on average, higher than the antidepressant trials!)
Again, it actually estimates a dose-response curve! Below is Figure 1 + Table 2, showing the effect of Vitamin D dosage on depression vs placebo. The solid line is the average estimated effect, dashed lines are 95% confidence interval. Note the effect size is negative in this figure, because they're measuring reduction in depressive symptoms:
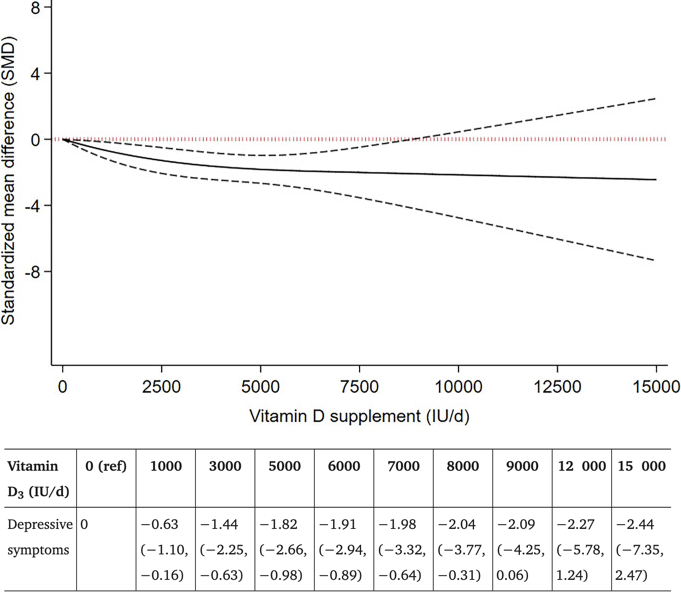
The upper range of uncertainty is lowest at 5000 IU (International Units) of Vitamin D a day, with an estimated effect size of 1.82, with a 95% uncertainty range, from 0.98 to 2.66. Let's be pessimistic, and take the lowest end: 0.98, like taking your mental health from an F to D, or C to B.
Is this in line with earlier meta-analyses? Again, more or less! Mikola et al 2022 found a lower estimate: the effect for ≥ 2000 IU/day is 0.407. Note that even this is still on par with the best antidepressant! And Xie et al 2022 found a higher estimate: the effect of > 2,800 IU/day is 1.23. So, I'll take the median estimate: around 0.98. (And I'm recommending 4,000 IU/day, since that's the "official" max safe dose. Though as we'll see later, even the official max dose may be too low.)
Is there "publication bias"? Ghaemi 2024 & Xie 2022 did NOT detect bias, Mikola 2022 did. (Again, meta-analyses differed in which studies met their quality criteria.) It's worth noting that Mikola, even adjusting for publication bias, even including low-dose studies, still finds an "average" effect of 0.317 — on par with the median antidepressant's 0.28. If we restrict ourselves to "just" high-dose Vitamin D, we get a much higher effect.
Does Vitamin D work long-term? Unknown, because of an important confounding variable: the shorter trials used higher doses, the longer trials used lower doses. Quote Mikola: "the mean vitamin D dose was more than 2,900 IU/day in interventions lasting 12 weeks or more, versus approximately 5,700 IU/day in shorter interventions." (Note that "12 weeks" is on par with traditional antidepressant trials.)
Does this still work even if you're already taking antidepressants? Yup! Table 1 of the Ghaemi meta-analysis, also shows that Vitamin D helps for both patients using antidepressant medication, and not. This is encouraging: it means you can stack both medications & supplements!
Does this still work even if you don't have Vitamin D insufficiency? Yes, but admittedly much less. That said, you probably do have a Vitamin D insufficiency. Liu et al 2018 finds that a bit under half of American adults (41.4%) have insufficient Vitamin D blood levels. And Manios et al 2017 finds that over half of kids (52.5%) in Greece — frickin' sunny Greece! — are still Vitamin D insufficient.
Also, the "official" recommendations are all too low:
So, if these three meta-analyses are right, then high doses — 2000 IU/day or more, possibly 4000 (official max dose) or higher — is optimal. But the official recommendation for Vitamin D is 400–800 IU/day, several times too low.
And even the official max dose of 4000 IU/day may be too low! But McCullough et al 2019 gave over thousands of participants 5,000 to 10,000 IU/day, for seven years, and there were zero cases of serious side effects. This matches later studies like Billington et al 2020, a 3-year-long trial on hundreds of participants, which found "the safety profile of vitamin D supplementation is similar for doses of 400, 4000, and 10,000 IU/day." (Although 15 participants got "mild hypercalcemia", but "all cases resolved on repeat testing." Either way, that's a small cost for reducing the risk of major depression & suicide.)
And it makes evolutionary sense that 10,000 IU a day should be safe. Your skin, exposed to the Sun's ultraviolet rays, can synthesize up to (the equivalent of) 10,000 IU a day, before plateauing out. Source is Vieth 1999: “Because vitamin D is potentially toxic, intake of [1000 IU/day] has been avoided even though the weight of evidence shows that the currently accepted [limit] of [2000 IU/day] is too low by at least 5-fold.” And Papadimitriou 2017 reviews several previous studies that find statistical errors behind official recommendations; correcting for these, adults should get 8000 IU/day.
(On the other hand, Krzyścin et al 2016 estimates that the existing hunter-gatherer group, the Hadza, get 2000 IU of Vitamin D from sun exposure, and their food is a poor source of Vitamin D. Given that existing hunter-gatherers live in the areas the colonialists didn't want, ancient hunter-gatherers probably ate & got more Vitamin D. So, 2000 IU is a lower bound on how much Vitamin D one should get — still several times more than the current official recommended dose of 400–800 IU/day.)
So why are all the official sources still so paranoid about Vitamin D, and lowballing the recommendations? Well, alas, official policy is always a few decades behind the science in any field. See: trans fats, open-label placebos, aerosol transmission of Covid-19, etc. And because something something incentives, it's "rational" for government/insurers to be very risk-averse & slow to change (for better & worse).
Speaking of the Sun, why take supplements instead of just getting Vitamin D from sun exposure? Well, skin cancer. But also: because Sun-Skin D varies greatly depending on the season, your latitude, and your skin type. There's less ultraviolet rays from the Sun in winter/fall, and at latitudes further from the equator. And the darker your skin is, the less Vitamin D your skin makes for the same amount of Sun exposure. As expected from the bio-physics of skin, Black adults have the highest prevalence of Vitamin D deficiency (82.1%!!), followed by Hispanic adults (62.9%). (But hey, at least Black adults have the lowest incidence of skin cancer. You win some you lose some.) The point is: speaking as someone with Southeast Asian skin, who's currently in Canada during winter... even if I stood outside naked for hours, I'd get approximately zero IU/day of Vitamin D from the Sun. Thus: supplements.
Direct effect on suicide: Finally, a meta-analysis directly measuring the effect of Vitamin D on suicidal behaviour. Yu et al 2025: “Vitamin D in patients with [suicidal behaviours] were significantly lower than in controls (standardized mean difference: –0.69, or a 'medium' difference)”. Reminder that this paper by itself only measures correlation, not causation — but combined with the above experiments of Vitamin D on depression, I think it's reasonable to guess it's partly causal.
To recap:
- Almost half of you have a Vitamin D insufficiency according to the official recommendation (800 IU/day).
- And those official recommendations are way too low. The optimal amount of Vitamin D for depression is probably 4000 IU/day, with an effect around twice that of the best antidepressant.
- Even the official maximum safe dose (4000 IU/day) is below what your body can produce from the Sun in optimal conditions (10,000 IU/day). Recent randomized controlled trials confirm that 10,000 IU/day is, indeed, mostly safe.
- Reminder that official policy is often decades behind the science.
- Reminder that I'm not saying "take supplements instead of antidepressants"; in fact the above meta-analysis shows you can effectively stack them!
Bonus: Vitamin D supplementation was found in several randomized controlled trials to reduce mortality from Covid-19, though much less than official treatments like Paxlovid. Vitamin D also probably helps guard against influenza too, though the evidence is small & early.
Conclusion: All this time, you lacked the Vitamin?
Scurvy is caused by a lack of Vitamin C. It's a condition that causes your wounds to re-open up & teeth to fall out. Scurvy used to kill almost half(!) of all sailors on major expeditions; it's estimated millions died. It can be cured by eating lemons.
Rickets is mostly caused by a lack of Vitamin D. It's a condition where kids' bones go all soft and deformed. During the Industrial Revolution, up to 80% of kids suffered from it. It can be prevented with cod liver oil.
Goiters is mostly caused by a lack of Iodine. It's a condition where the thyroid gland in your neck swells up painfully, to the size of an apple. During WWI, a third of adult men had goiters. It can be prevented with iodized salt.
About 1 in 4 people are expected to have clinical depression sometime in their life. Depression is the #1 source of the global "burden from disease" in the mental health category, and that category is the #6 burden of disease in the world, above Alzheimer's, malaria, and sexually transmitted infections.
(But honestly, did you need those stats? This is likely a lived experience for a lot of you reading this.)
The effective altruists are all, "woah for just $3000 you can prevent a child's death from malaria" — and that's great! save them kids! — but where's the fanfare for the accumulating evidence that, "woah with cheap daily supplements we can save millions from suicide & depressed lives"?
Over and over again throughout history, some horrific thing that caused millions to suffer, turned out to be "yeah you were missing this one molecule lol". To be clear: not everything is gonna be that simple, and mental health is not "just" chemistry. Also, all the numbers on this page have with large error bars & uncertainty, more research is needed.
But, as of right now, I feel I can at least confidently claim the following:
- Vitamin D and Omega-3 are both at least on par with the median antidepressant (effect size ~= +0.3).
- The evidence is much stronger for Vitamin D; it's very plausibly at least twice as good as antidepressants.
- Both supplements are cheap and safe, so what's the harm of trying? (positive "expected value" for this bet)
So:
MY RECOMMENDATIONS FOR RESEARCHERS:
More big, pre-registered, double-blind randomized controlled trials, please. (And specifically: testing high doses.)
MY SPECIFIC RECOMMENDATIONS FOR YOU:
- Go to a pharmacy, buy the following supplements over-the-counter, in whatever form you like: (I like the easy-to-swallow gel capsules)
- Vitamin D
- 🌱 By default, Vitamin D supplements are derived from… (quick web search)… the grease in sheep's wool? Huh. Also fish liver oil. Anyway, if you're vegan, make sure your bottle specifically says "vegan" or "from lichen/mushrooms". (If you're vegetarian, the sheep's-wool Vitamin D is fine, they don't kill the sheep for it.)
- Omega-3 where EPA is ~60% of the Omega-3 total. For example, my 500mg Omega-3 capsules have 300mg EPA, 200mg DHA.
- 🌱 By default, Omega-3 supplements come from fish. If you're veg(etari)?an, there are plant-based sources of Omega-3, but look carefully: most vegan Omega-3 supplements provide more DHA than EPA, which the above studies suggest fully cancel out the antidepressant effect. Double check the nutritional label to make sure it's ≥60% EPA. For example, this one is 300mg EPA + 200mg DHA. (not an affiliate link)
Then, every day:
- Take ~4000 IU of Vitamin D
- ⚠️ be cautious if you have kidney stones, or are on medications that could interact with Vitamin D. "ask your doctor".
- (4,000 IU is the official max safe dose)
- 10,000 IU if you're feeling daring (a couple large controlled trials showed no major lasting adverse side effects).
- if you have darker skin / live in higher latitudes / it's winter, you definitely need some form of vit D supplementation
- bonus: may improve immune response to Covid & influenza?
- Take ~1500 mg of ≥60%-EPA Omega-3
- ⚠️ be cautious if you're on blood thinners, or other medications that could interact with Omega-3. again, "ask your doctor".
- (5000 mg/day is the official max safe dose)
- bonus: may improve cognition?
- Don't quit your existing antidepressants if they're net-positive for you!
- you may also want to ask your doctor about Amitriptyline, or those other best-effect-size antidepressants.
Can you get these doses of Vitamin D & Omega-3 through whole foods alone, no supplements? Probably, but it'd be expensive & tedious: you'd have to eat something like 2,000 calories of farmed salmon a day to get 4,000 IU/day of Vitamin D. As for Omega-3, eating mostly oily fishes would get you >1000mg of Omega-3, but they'd be more DHA than EPA, which the above studies suggest would cancel out the antidepressant effects.
The effect sizes on depression:
- The best antidepressant: +0.417
- like your mental health grade going from F to F+, or C to C+
- 1500mg of ≥60%-EPA Omega-3: +0.558
- like your mental health grade going from F to D–, or C to B–
- 4000 IU of Vitamin D: +0.98
- like your mental health grade going from F to D, or C to B
For completeness & comparison, here's the effect size of other things on depression:
- Any mainstream "bona-fide" psychotherapy (CBT, Psychodynamic, Humanist, Solutions-Focused): +0.35, source: Kamenov et al 2016
- like going from C to C+
- Aerobic/Cardio Exercise: +0.79, source Ioannis et al 2018
- like going from C to B–
- (dose: "45 minutes, at moderate intensity, three times/week" ⇒ ~20 min/day)
- Good Sleep: +1.10(???), a lot of interpretation & calculations, see footnote[5]
- like going from C to B
- (dose: going from moderate insomnia to healthy sleep)
- Bright Light Therapy: +0.487, source Menegaz de Almeida et al 2025
- (the above paper reports Odds Ratio of 2.42, which converts to Cohen's d effect size of +0.487)
- like going from C to C+
- I went with Wirecutter's recommendation for a UV-free 10,000 lux lamp.
- (dose: 10,000 lux, 30 min a day)
- Mindfulness Meditation: +0.42, source Breedvelt et al 2019
- like going from C to C+
- (dose: 7 weeks, "153 min each week" ⇒ ~20 min/day)
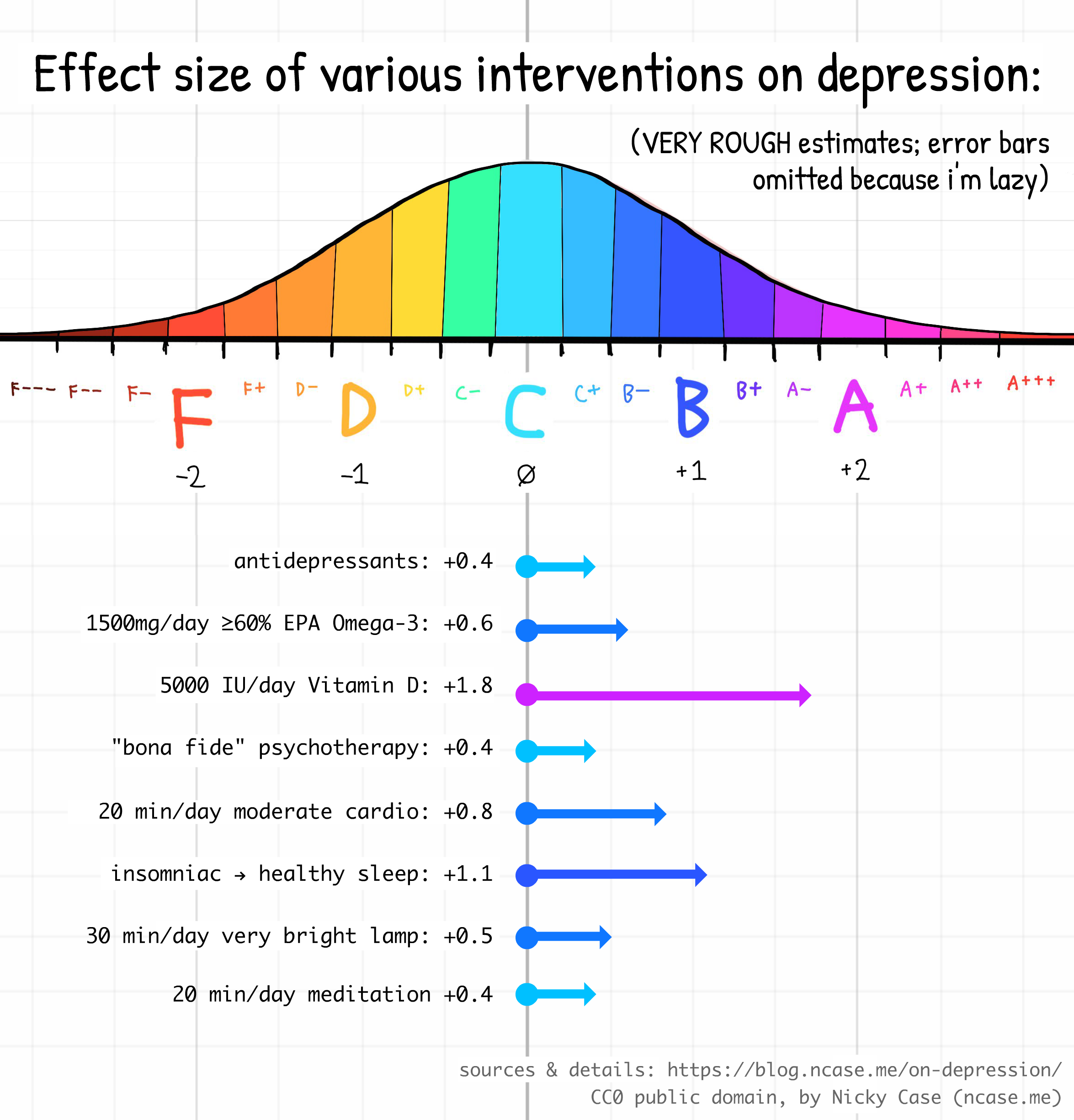
(And remember to add +0.4 for the power of hope, e.g. "placebo"! Also remember: you can stack any of the above interventions to get an even larger effect! You can't just naively add up the effect sizes, but I'd be surprised if the effect of {vitamin d + omega-3 + bright lamps + cardio + good sleep + meditation + therapy + antidepressants} combined ends up being less than +2.00. Two letter grades up means going from D to B, or, theoretically, from clinically depressed to flourishing! For more papers & my working research notes on "best bang for buck on depression", check out this Google Doc.)
Also, remember that all the above estimates are uncertain. And that averages hide variation in effect. That said, I still think the overall picture is still strong: there exist high bang-for-buck ways to reduce depression, which are at least on par with drugs & therapy (and plausibly 2x better), that aren't (yet) common knowledge amongst policymakers & the public. And again, they're dirt cheap with minor-to-no adverse side effects. Moderate chance of a big win, for a known tiny cost. That's a positive "expected value" bet right there.
I got onto this research rabbithole a few months ago while borrowing my housemate's ADHD meds, which I may or may not eventually collect into a "JOYMAXXING" informal meta-meta-analysis. (: See me yap about it on video as a cartoon cat.) But for this blog post, I wanted to dive deeper into Vitamin D and Omega-3, since their effect sizes are so huge, and they're insultingly cheap & easy, compared to therapy or regular cardio.
Stay safe this winter, keep away the seasonal depression. Get your supplements, and reach out to your friends & loved ones!
💖,
~ Nicky Case
I made up these ranges by requiring the standard letter grades F,D,C,B,A, to have their centers be -2,-1,0,+1,+2. Then, I made sure all in-between grades like C+ or A– had equal intervals. Each interval is +/- ⅙, or ⅓ wide:
- F---: -3.16 to -2.83
- F--: -2.82 to -2.50
- F–: -2.49 to -2.17
- F: -2.16 to -1.83
- F+: -1.82 to -1.50
- D–: -1.49 to -1.17
- D: -1.16 to -0.83
- D+: -0.82 to -0.50
- C–: -0.49 to -0.17
- C: -0.16 to +0.17
- C+: +0.18 to +0.50
- B–: +0.51 to +0.83
- B: +0.84 to +1.17
- B+: +1.18 to +1.50
- A–: +1.51 to +1.83
- A: +1.84 to +2.17
- A+: +2.18 to +2.50
- A++: +2.51 to +2.83
- A+++: +2.84 to +3.17
Median antidepressant Odds Ratio: 1.66, see below figure. This converts to Cohen's d of 0.279. ↩︎
See Fountoulakis & Möller 2011 Table 1 Row 2. Will talk more about this paper again in a few paragraphs. ↩︎
See Table 1. A follow-up paper by Kirsch in in 2008 found that the drug group improved by 9.60 (non-standardized) points, and the placebo group by 7.80 points. (So, placebo + time is 7.80/9.60 = 0.81 = 81% of the full effect.) The F&M recalculation found the drug group improved by 10.04 points, and the placebo by 7.85 points. (So, placebo + time is 7.85/10.04 = 0.78 = 78% of the full effect.) And rows 2 & 3 confirm that Kirsch was still right about the following: “The [total effect] for drug groups was 1.24 [C to B+] and that for placebo 0.92 [C to B]” and “The effect size concerning the difference between improvement in drug groups and improvement in placebo groups was 0.32 [like C to C+]”. ↩︎
Lee et al 2023 reports the following effect sizes. Digital therapy for Insomnia → Sleep = 0.76, and Digital therapy for Insomnia → Depression = 0.42. Assuming the therapy for insomnia specifically affects depression only through better sleep (Digital therapy for Insomnia → Sleep → Depression), we can do an "Instrumental Variable" estimate of the effect of Sleep → Depression = 0.42 / 0.76 = 0.55. To be precise: this is saying, if you improve your sleep by 1 standard deviation, on average your depression improves by 0.55 standard deviations.
So: how many standard deviations is going from "moderate insomnia" to "healthy sleep"? The standard measure is the Insomnia Severity Index (ISI), which you can take online. A score of 0–7 means no insomnia, 8–14 is subclinical insomnia, 15–21 is clinical insomnia (moderate), 22–28 is clinical insomnia (severe). Let's be conservative and say we're just going from barely clinical to barely healthy: 15 to 7, or a reduction of 8 points. Yang et al 2009 says a 6-point reduction is 1.5 standard deviations, which means 4 points is 1 standard deviation. So a reduction of 8 points is 2 standard deviations. So, if you improve your sleep from insomniac to healthy, you improve by at least 8 points, which is 2 standard deviations, so your depression should improve by 2 × 0.55 standard deviations, or ~1.10.
Reminder that my estimate is full of assumptions upon assumptions & these error bars will compound. But I'd be surprised if the true causal effect of going from insomniac to healthy sleep isn't at least a "large" +0.8 effect. ↩︎